Mitral Valve Prolapse, FDA device approval, connective tissue disorder, genetics, Vitamin C
FDA, the progenitors of "Alternative Medicine"
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8114626/
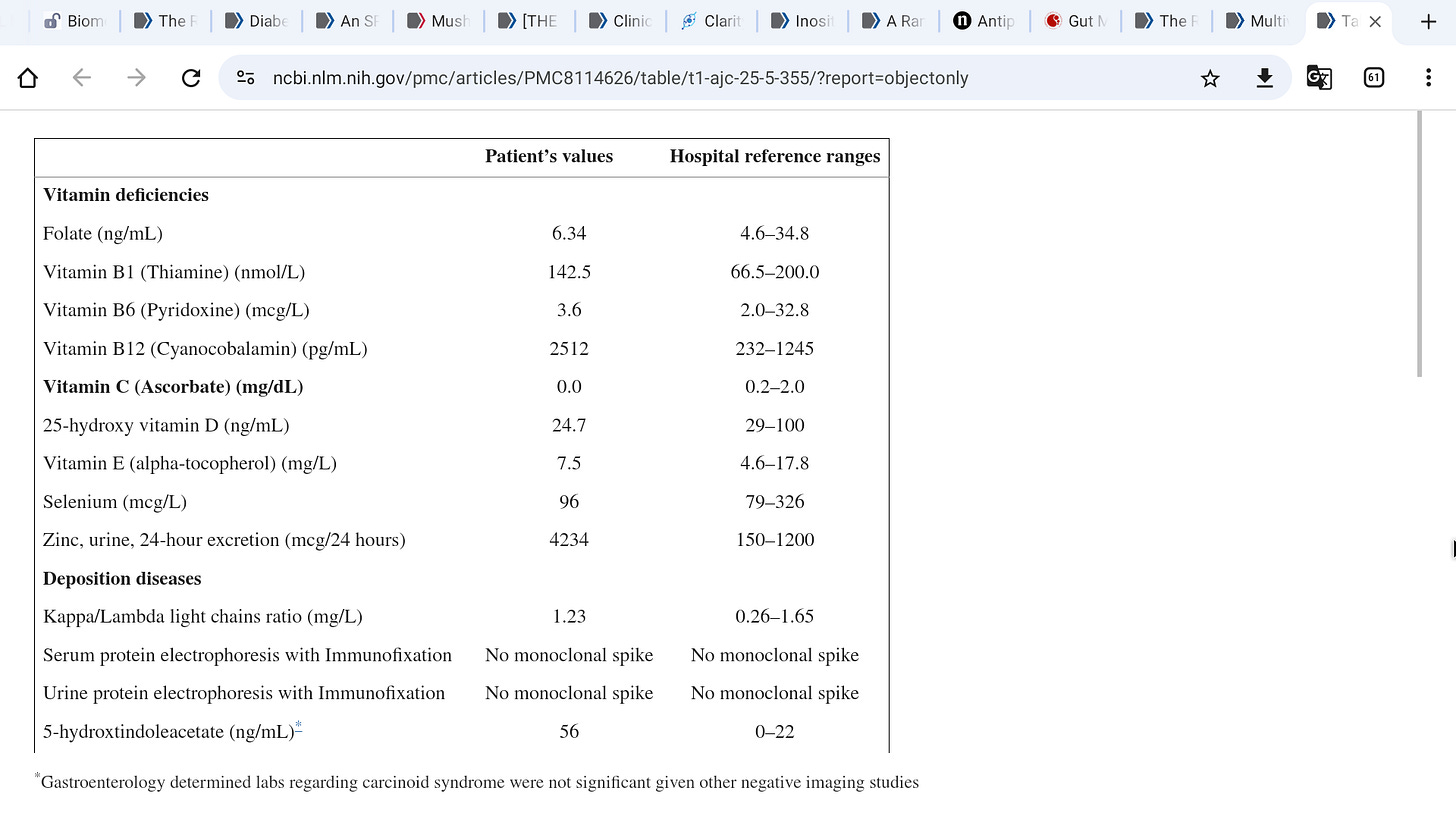
»Further workup did not demonstrate other vitamin deficiencies, liver disease, infection, heavy metal toxicity, carcinoid syndrome, amyloidosis, sarcoidosis, or autoimmune diseases (Table 1). Pulmonary embolism and coronary artery disease were ruled out with CT angiography and invasive coronary angiography. Further history taking revealed no evidence of prior endocarditis, supplement, or drug use. Right heart catheterization demonstrated elevated left- and right-sided pressures, with an right atrium (RA) pressure of 20 mm Hg, mean pulmonary artery pressure of 35 mm Hg, mean pulmonary capillary wedge pressure of 16 mm Hg, and cardiac index of 2.1 L/min/m2 using the Fick equation.«
Nowhere on the AHA web page dedicated to MVP is magnesium mentioned, nor vitamin c, nor specialized pro resolving Mediators, nor Omega 3’s, Pycnogenol, etc.
»It is concluded that many patients with heavily symptomatic MVP have low serum magnesium, and supplementation of this ion leads to improvement in most symptoms along with a decrease in catecholamine excretion.«
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6616454/
Endothelial Dysfunction in Patients with Severe Mitral Regurgitation
Abstract
Mitral valve prolapse (MVP) is the most common cause of severe mitral regurgitation. It has been reported that MVP patients—candidates for mitral valve repair (MVRep)—showed an alteration in the antioxidant defense systems as well as in the L-arginine metabolic pathway.
In this study, we investigate if oxidative stress and endothelial dysfunction are an MVP consequence or driving factors. Forty-five patients undergoing MVRep were evaluated before and 6 months post surgery and compared to 29 controls.
Oxidized (GSSG) and reduced (GSH) forms of glutathione, and L-arginine metabolic pathway were analyzed using liquid chromatography-tandem mass spectrometry methods while osteoprotegerin (OPG) through the ELISA kit and circulating endothelial microparticles (EMP) by flow cytometry.
Six-month post surgery, in MVP patients, the GSSG/GSH ratio decreased while symmetric and asymmetric dimethylarginines levels remained comparable to the baseline.
Conversely, OPG levels significantly increased when compared to their baseline. Finally, pre-MVRep EMP levels were significantly higher in patients than in controls and did not change post surgery.
Overall, these results highlight that MVRep completely restores the increased oxidative stress levels, as evidenced in MVP patients.
Conversely, no amelioration of endothelial dysfunction was evidenced after surgery. Thus, therapies aimed to restore a proper endothelial function before and after surgical repair could benefit MVP patients.
Keywords: glutathione, osteoprotegerin, oxidative stress, endothelial microparticles, mitral valve prolapse